Anal fistula surgery can be a necessary step for patients experiencing chronic discomfort, recurrent infections, or complications from an anal fistula. Understanding what to expect during recovery is essential to reduce anxiety and support proper healing. Recovery experiences can vary depending on the type of surgery, overall health, and adherence to post-operative care instructions. Common procedures for anal fistula repair and removal include fistulotomy, fistulectomy, and sphincter-sparing techniques. Each of these approaches has its own recovery timeline and specific care requirements. Patients often have questions about pain management, wound care, and the timeline for returning to normal activities. Being informed ahead of time can make the recovery process smoother and more predictable.
Understanding Anal Fistula Surgery
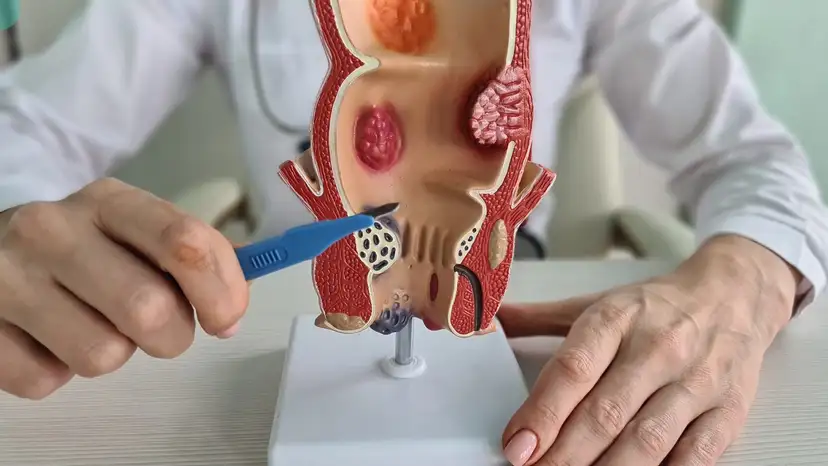
Anal fistulas are abnormal tunnels connecting the inside of the anus to the skin surrounding it. Surgery aims to remove the fistula while preserving anal sphincter function. Fistulotomy involves cutting open the fistula tract and allowing it to heal from the inside out, which usually has a shorter recovery period. Fistulectomy involves complete removal of the fistula tract, which can result in a larger wound and potentially longer healing. Sphincter-sparing techniques are designed to reduce the risk of incontinence while promoting healing. The type of surgery performed directly impacts pain levels, recovery duration, and follow-up care. Patients should discuss their individual case with a colorectal surgeon to understand which procedure is most appropriate.
Immediate Post-Surgery Recovery
The first 24 to 48 hours after surgery are typically the most uncomfortable. Pain, swelling, and mild bleeding are common during this period. Pain management is crucial and can include prescription medications, over-the-counter pain relievers, or topical ointments recommended by a doctor. Sitz baths, which involve sitting in warm water, can help reduce discomfort and promote blood flow to the surgical site. Patients should follow their surgeon’s instructions regarding wound care and hygiene. Keeping the area clean and dry, changing dressings as directed, and monitoring for signs of infection are all important. Most patients are advised to rest and avoid strenuous activity during these initial days.
First Few Weeks: Healing Progress
Recovery progresses gradually in the weeks following surgery. The wound typically begins to heal from the inside out, which can take several weeks depending on the procedure. Patients may experience minor discomfort, swelling, or occasional bleeding during this period. Activity should be limited, including avoiding heavy lifting, prolonged sitting, or vigorous exercise. A high-fiber diet, hydration, and stool softeners are often recommended to reduce strain during bowel movements. Sitz baths can continue to be used multiple times per day to ease discomfort and aid healing. It is essential to watch for unusual symptoms such as fever, increasing pain, or foul-smelling discharge, which could indicate infection or complications.
Pain and Swelling Management
- Use prescribed pain medications exactly as instructed.
- Warm sitz baths for 10–15 minutes several times daily.
- Keep the surgical area clean and dry to reduce irritation.
- Wear loose-fitting clothing to avoid friction.
- Avoid prolonged sitting or pressure on the surgical site.
- Monitor bowel movements and use stool softeners to prevent straining.
- Contact your doctor immediately if swelling or bleeding worsens.
Managing discomfort effectively during this stage can significantly improve the overall recovery experience. It also helps reduce the risk of complications and promotes faster healing.
Long-Term Recovery Expectations
Complete recovery varies based on the type of surgery performed. For fistulotomy, patients may experience healing within 4 to 6 weeks, while fistulectomy may take up to 8 to 12 weeks due to larger wounds. Sphincter-sparing procedures may also require longer recovery, especially if multiple tracts are involved. Returning to work and daily routines depends on individual healing rates and the physical demands of the patient’s job. Resuming physical activity should be gradual, starting with light movements and progressing as tolerated. Sexual activity should only resume when the area is fully healed and pain-free. Some patients may experience minor incontinence or recurrence, which should be discussed with the surgeon during follow-up visits.
Maintaining Hygiene and Preventing Complications
Proper hygiene is critical for preventing infection and supporting healing. Gently cleaning the area with warm water after bowel movements can prevent irritation and bacterial buildup. Patients should avoid using harsh soaps or chemicals that may damage sensitive tissues. Dressing changes should follow the surgeon’s instructions carefully, and wound care supplies should be kept sterile. Lifestyle adjustments, such as maintaining a high-fiber diet and staying hydrated, can reduce strain on the surgical site. Avoiding constipation and prolonged sitting will help prevent pressure on the wound. Regular monitoring for signs of infection or recurrence is essential for long-term recovery. Patients should feel empowered to ask their surgeon for guidance on any issues that arise.
Follow-Up Care and Monitoring
Follow-up appointments allow surgeons to monitor healing and address potential complications. The doctor may inspect the wound, check for signs of infection, and evaluate the integrity of the anal sphincter. Imaging or other tests may occasionally be recommended if there are concerns about recurrence. Additional procedures may be necessary in rare cases if the fistula does not heal completely. Patients should report persistent pain, unusual bleeding, or changes in bowel habits promptly. Communication with the healthcare team ensures that any issues are addressed early. Regular follow-up is a key component of successful recovery after anal fistula surgery.
Frequently Asked Questions
- How long does it take to fully recover from anal fistula surgery?
Recovery depends on the type of surgery, but most patients heal within 4 to 12 weeks. - Will I experience pain during bowel movements after surgery?
Mild discomfort is common, but stool softeners and proper hygiene can minimize pain. - Are there activities I should avoid to prevent recurrence?
Avoid heavy lifting, prolonged sitting, and strenuous exercise until cleared by your doctor. - Can anal fistula surgery affect continence?
Minor incontinence is possible, especially with more invasive procedures, but most patients regain full control. - How can I reduce the risk of infection after surgery?
Follow wound care instructions, keep the area clean, and use sitz baths as recommended. - Is recurrence common, and what factors increase the risk?
Recurrence can occur in complex or untreated fistulas; early treatment and proper post-operative care help reduce risk. - When should I contact my doctor for complications?
Seek medical attention for worsening pain, persistent bleeding, foul discharge, fever, or delayed healing.
Takeaway
Recovery expectations after anal fistula surgery vary depending on the type of procedure and individual health. Immediate post-surgery care, proper pain management, hygiene, and adherence to follow-up appointments are essential for smooth healing. Patients can expect gradual improvement in pain and swelling over the first few weeks, with a return to normal activities in a safe, progressive manner. Maintaining a high-fiber diet, staying hydrated, and following surgeon instructions help reduce complications and recurrence. Open communication with a colorectal surgeon ensures that recovery is monitored effectively, and any issues are addressed promptly. Understanding the recovery process helps patients regain confidence, comfort, and long-term anal health.